In Focus: Clinical Subtypes of Misophonia in Youth
In Focus: Clinical Subtypes of Misophonia in Youth
By Gabrielle M. Armstrong, BA, University of Mississippi
Ogechi C. Onyeka, PhD, Baylor College of Medicine
Eric A. Storch, PhD, Baylor College of Medicine
Andrew G. Guzick, PhD, University of Pennsylvania
Misophonia is a chronic condition characterized by intense intolerance to specific auditory stimuli typically produced by other people, which may include food chewing, breathing, or pen clicking (Lewin et al., 2021; Schröder et al., 2013; Swedo et al., 2022). Although the diagnostic traits of misophonia are heterogeneous, individuals with this condition share key phenotypic features, including significant emotional distress in response to triggers as well as intense physiological and behavioral reactions such as muscle tension, sensory overwhelm, aggression, or escape behavior (Cavanna & Seri, 2015; Edelstein et al., 2013; Schröder et al., 2013). While early research surrounding misophonia was largely delineated by case studies and observational reports (Schneider & Arch, 2017; Schröder et al., 2013), more recent studies have begun to uncover its underlying mechanisms (Rosenthal et al., 2023; Kumar et al., 2021). Despite these advances, a detailed understanding of misophonia and its clinical presentation, particularly in youth, remains unclear.
Is Misophonia a Standalone Condition or Part of a Larger Phenomenon?
The classification of misophonia is a topic of ongoing debate in the literature. While extant research suggests that misophonia may manifest as a distinct, standalone condition (Rosenthal et al., 2022), others indicate that the clinical profiles of misophonia often include a complex interplay of co-occurring psychological or neurophysiological phenomena (Ferrer-Torres & Giménez-Llort, 2022; Guzick et al., 2023; McKay et al., 2018; Wu et al., 2014). These overlapping features complicate efforts to accurately capture the full clinical picture of misophonia and may point to the existence of distinct subtypes of the condition. For example, many individuals with misophonia often share characteristics with various internalizing disorders, such as disgust sensitivity, emotion regulation difficulties, and intense reactions to specific stimuli (Barahmand et al., 2021; Claiborn et al., 2020; Dixon et al., 2024). Additionally, the aggressive reactions observed in misophonia often overlap with behaviors commonly associated with externalizing disorders (Guzick et al., 2023; Ferrer-Torres & Giménez-Llort, 2022), with some evidence suggesting an association between these behaviors and sensory sensitivities (Armstrong et al., 2023). The coexistence of these symptoms suggests that misophonia may manifest differently across individuals, making it challenging to define precise clinical characteristics. This variability in clinical profiles highlights the need for more nuanced diagnostic methods and personalized treatment approaches. Furthermore, while some studies have explored distinct profiles of misophonia in adult community samples (McKay et al., 2018), few have done so with clinical samples, and there is a notable absence with youth samples. Retrospective studies suggest that misophonia typically begins in childhood or adolescence (Clairborn et al., 2020; Jager et al., 2020) and is linked to considerable impairment and distress across various areas of life (Remmert et al., 2022; Rinaldi et al., 2022). This gap is particularly concerning, as early identification and intervention could be crucial for mitigating long-term psychological or social impacts of misophonia. Therefore, further investigation into the clinical diversity of misophonia in youth and various diagnostic contexts is critical for developing more effective and targeted treatment strategies.
Understanding Clinical Subtypes of Misophonia in Youth: Insights from Our Recent Study
We aimed to explore the presence of clinical subtypes of misophonia in youth. Our goal was to better understand how misophonia presents in young people and whether distinct subtypes would be identified based on symptom severity and co-occurring psychopathology.
We collected data from 102 youth (Mage = 13.71) who met the clinical threshold for misophonia. Participants completed a series of validated assessments that measured misophonia severity and impact, internalizing and externalizing symptoms, and sensory sensitivity—in line with previous research demonstrating their respective associations with misophonia symptom severity (Guzick et al., 2023; Rinaldi et al., 2022). Additionally, we gathered demographic characteristics and a validated assessment of quality of life, comparing these factors across different clusters identified in the data. A hierarchical agglomerative cluster analysis was conducted to examine the natural groupings across variables, which was then validated by a k-means cluster analysis.
Results indicated three distinct groups:
- High Externalizing Symptoms, High Symptom Severity Group: Youth who exhibit strong emotional reactions, often expressed outwardly, with elevated symptom severity
- Pure Misophonia, Low Symptom Severity Group: Youth primarily affected by misophonia with minimal overall symptom severity
- High Internalizing Symptoms, High Sensory Sensitivity Group: Youth experiencing high levels of internalizing symptoms (e.g., depression and anxiety) and elevated sensitivity to sensory stimuli
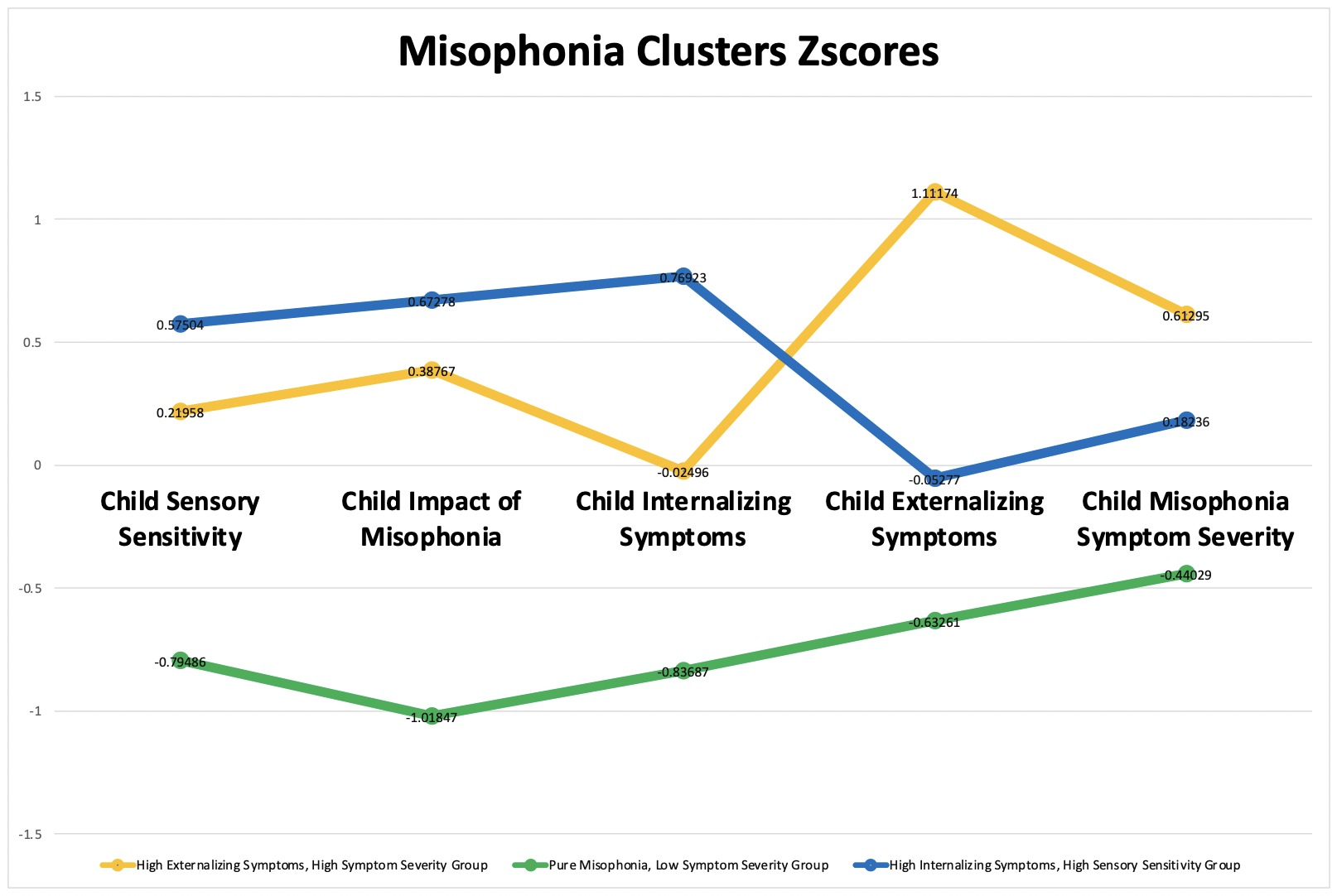
Interestingly, while the groups did not differ by gender, there was a statistically significant difference in age. Youth in the Pure Misophonia, Low Symptom Severity group were the youngest, which may suggest that misophonia symptoms become more pronounced or co-occur with other psychopathology as children age. Additionally, a significant difference was observed in child-reported quality of life. Youth in the Pure Misophonia, Low Symptom Severity group reported the highest levels of quality of life, indicating that less severe symptoms may be less disruptive to their daily functioning and overall well-being.
Implications for Treatment and Support
Our findings suggest that misophonia is not a one-size-fits-all condition. Instead, there may be subtypes representing clinical profiles characterized by severity and comorbidity. The identification of these subtypes is crucial for developing effective, tailored treatment approaches. For example, individuals in the High Internalizing Symptoms, High Sensory Sensitivity group may benefit from therapies targeting anxiety and sensory processing, while those in the High Externalizing Symptoms, High Symptom Severity group may require interventions focused on emotion regulation and behavior management.
This variability also emphasizes the importance of early intervention. While youth in the Pure Misophonia, Low Symptom Severity group may experience fewer disruptions in daily life, they also appeared younger, and thus it may be that early intervention is key to help offset trajectories that corresponds with increasing severity and more comorbidity. Those in the more severe groups may also benefit from earlier, targeted support to manage the emotional and behavioral difficulties associated with misophonia. By recognizing the spectrum of misophonia and its varied clinical presentations, clinicians can tailor treatment strategies to meet the specific needs of each individual, improving the overall effectiveness of care. As research continues to evolve and treatment approaches become more refined, the emotional and social well-being of youth with misophonia is expected to improve, ultimately supporting them in leading more fulfilling lives.
References
Armstrong, G. M., Greenberg, R. L., Smárason, O., Frederick, R. M., Guzick, A. G., Schneider, S. C., Spencer, S. D., Cervin, M., & Storch, E. A. (2023). Factors associated with internalizing and externalizing symptoms in a clinical sample of youth with misophonia. Journal of Obsessive-Compulsive and Related Disorders, 39, 100831. https://doi.org/10.1016/j.jocrd.2023.100831
Barahmand, U., Stalias-Mantzikos, M.E., Rotlevi, E., & Xiang, Y. (2021). Disgust and Emotion Dysregulation in Misophonia: a Case for Mental Contamination? International Journal of Mental Health and Addiction, 21, 1550-1569.
Cavanna, A. E., & Seri, S. (2015). Misophonia: Current perspectives. Neuropsychiatric Disease and Treatment, 11, 2117–2123. https://doi.org/10.2147/NDT.S81438
Claiborn, J. M., Dozier, T. H., Hart, S. L., & Lee, J. (2020). Self-identified misophonia phenomenology, impact, and clinical correlates. Psychological Thought, 13(2), 349 – 375. doi: 10.37708/psyct.v13i2.454
Dixon, L. J., Sevier, C. J., & Freshley, A. M. (2024). Emotion dysregulation in misophonia: Findings from a nationally representative sample. Journal of Psychiatric Research, 180, 266–272. https://doi.org/10.1016/j.jpsychires.2024.10.022
Edelstein, M., Brang, D., Rouw, R., & Ramachandran, V. S. (2013). Misophonia: physiological investigations and case descriptions. Frontiers in Human Neuroscience, 7, 296. https://doi.org/10.3389/fnhum.2013.00296
Ferrer-Torres, A., & Giménez-Llort, L. (2022). Misophonia: A Systematic Review of Current and Future Trends in This Emerging Clinical Field. International Journal of Environmental Research and Public Health, 19(11), Article 11. https://doi.org/10.3390/ijerph19116790
Guzick, A. G., Cervin, M., Smith, E. E. A., Clinger, J., Draper, I., Goodman, W. K., Lijffijt, M., Murphy, N., Lewin, A. B., Schneider, S. C., & Storch, E. A. (2023). Clinical characteristics, impairment, and psychiatric morbidity in 102 youth with misophonia. Journal of Affective Disorders, 324, 395–402. https://doi.org/10.1016/j.jad.2022.12.083
Jager, I. J., de Koning, P., Bost, T., Denys, D., & Vulink, N. (2020). Misophonia: Phenomenology, comorbidity, and demographics in a large sample. PLoS ONE, 15(4), e0231390. https://doi.org/10.1371/journal.pone.0231390
Kumar, S., Dheerendra, P., Erfanian, M., Benzaquén, E., Sedley, W., Gander, P. E., Lad, M., Bamiou, D. E., & Griffiths, T. D. (2021). The Motor Basis for Misophonia. The Journal of Neuroscience, 41(26), 5762–5770. https://doi.org/10.1523/JNEUROSCI.0261-21.2021
Lewin, A. B., Dickinson, S., Kudryk, K., Karlovich, A. R., Harmon, S. L., Phillips, D. A., Tonarely, N. A., Gruen, R., Small, B., & Ehrenreich-May, J. (2021). Transdiagnostic cognitive behavioral therapy for misophonia in youth: Methods for a clinical trial and four pilot cases. Journal of Affective Disorders, 291, 400–408. https://doi.org/10.1016/j.jad.2021.04.027
McKay, D., Kim, S.-K., Mancusi, L., Storch, E. A., & Spankovich, C. (2018). Profile Analysis of Psychological Symptoms Associated With Misophonia: A Community Sample. Behavior Therapy, 49(2), 286–294. https://doi.org/10.1016/j.beth.2017.07.002
Remmert, N., Jebens, A., Gruzman, R., Gregory, J., & Vitoratou, S. (2022). A nomological network for misophonia in two German samples using the S-Five model for misophonia. Frontiers in Psychology, 13, 902807. doi: 10.3389/fpsyg.2022.902807
Rinaldi, L. J., Smees, R., Ward, J., & Simner, J. (2022). Poorer well-being in children with misophonia: Evidence from the Sussex Misophonia Scale for adolescents. Frontiers in Psychology, 13, 808379. doi: 10.3389/fpsyg.2022.808379
Rosenthal, M. Z., Campbell, J., & Altimus, C. (2023). Editorial: Advances in understanding the nature and features of misophonia. Frontiers in Neuroscience, 17, 1267682. https://doi.org/10.3389/fnins.2023.1267682
Rosenthal, M. Z., McMahon, K., Greenleaf, A. S., Cassiello-Robbins, C., Guetta, R., Trumbull, J., Anand, D., Frazer-Abel, E. S., & Kelley, L. (2022). Phenotyping misophonia: Psychiatric disorders and medical health correlates. Frontiers in Psychology, 13, 941898. https://doi.org/10.3389/fpsyg.2022.941898
Schröder, A., Vulink, N., & Denys, D. (2013). Misophonia: Diagnostic criteria for a new psychiatric disorder. PloS one, 8(1): e54706. https://doi.org/10.1371/journal.pone.0054706
Schneider, R. L., & Arch, J. J. (2017). Case study: A novel application of mindfulness- and acceptance-based components to treat misophonia. Journal of Contextual Behavioral Science, 6(2), 221–225. https://doi.org/10.1016/j.jcbs.2017.04.003
Swedo, S. E., Baguley, D. M., Denys, D., Dixon, L. J., Erfanian, M., Fioretti, A., Jastreboff, P. J., Kumar, S., Rosenthal, M. Z., Rouw, R., Schiller, D., Simner, J., Storch, E. A., Taylor, S., Werff, K. R. V., Altimus, C. M., & Raver, S. M. (2022). Consensus Definition of Misophonia: A Delphi Study. Frontiers in Neuroscience, 16, 841816. https://doi.org/10.3389/fnins.2022.841816
Wu, M. S., Lewin, A. B., Murphy, T. K., & Storch, E. A. (2014). Misophonia: Incidence, phenomenology, and clinical correlates in an undergraduate student sample. Journal of Clinical Psychology, 70(10), 994–1007. https://doi.org/10.1002/jclp.22098

Gabrielle M. Armstrong, BA
University of Mississippi

Ogechi C. Onyeka, PhD
Baylor College of Medicine

Eric A. Storch, PhD
Baylor College of Medicine

Andrew G. Guzick, PhD
University of Pennsylvania
“…early identification and intervention could be crucial for mitigating long-term psychological or social impacts of misophonia. Therefore, further investigation into the clinical diversity of misophonia in youth and various diagnostic contexts is critical for developing more effective and targeted treatment strategies.”
More From Summer 2025
More From Summer 2025
President’s Message
By Regine Galanti, PhD
In Focus: Clinical Subtypes of Misophonia in Youth
By Gabrielle M. Armstrong, BA, Ogechi C. Onyeka, PhD, Eric A. Storch, PhD, &, Andrew G. Guzick, PhD
Expert Recommendations: From Science to Advocacy
By Mary Ann McCabe, PhD, ABPP
The Student View: SCCAP Student Development Committee Updates
By Hong Bui & Sarah Kim
EPCAMH Journal Update
By Mary A. Fristad, PhD, ABPP
The SCCAP Conference Recap
By Mary Louise Cashel, PhD
SCCAP at APA 2025
By Kelsie Okamura, PhD & Sarah Dickinson, PhD
Science & Practice Committee Update
By Jennifer L. Hughes, PhD, MPH
Diversity Committee Update
By Juventino Hernandez Rodriguez, PhD
Membership Committee Update
By Nicole Lorenzo, PhD
Fellows Committee Update
By Martha C. (Marcy) Tompson, PhD
Distinguished Career Contributions to Science Award
Recipient: Mitch Prinstein, PhD, ABPP
Distinguished Career Award for Practice & Training
Recipient: Jonathan Weinand, PhD
Richard “Dick” Abidin Early Career Award
Recipient: Justin Parent, PhD
R. Bob Smith, III Excellence in Psychological Assessment Award
Recipient: Randall T. Salekin, PhD
Early Career Contributions to Diversity Science Award
Recipient: Roberto Luis Abreu, PhD
2025 Diversity Professional Development Awards
Eleven Winners Announced
2025 Routh Award Winners
Three Winners Announced
Student Achievement Award Winners
Six Winners Announced
2025 Student Development Committee Professional Development Awards
Five Winners Announced
AIRS SIG Update
By Elizabeth Frazier, PhD
Introducing The Autism Spectrum Disorder SIG
By Mariel Cannady, PsyD, NCSP & Allison Sallee, PhD
Bilingual Psychologists SIG Update
By Erika Garcia-Rocha, PsyD
Clinical Child & Adolescent Practice SIG Update
By Megan Lawson, PsyD, ABPP
Summer Treatment Program SIG Update
By Katie Hart, PhD & Sarah Tannenbaum, PsyD, ABPP
More From Summer 2025
More From Summer 2025
President’s Message
By Regine Galanti, PhD
In Focus: Clinical Subtypes of Misophonia in Youth
By Gabrielle M. Armstrong, BA, Ogechi C. Onyeka, PhD, Eric A. Storch, PhD, &, Andrew G. Guzick, PhD
Expert Recommendations: From Science to Advocacy
By Mary Ann McCabe, PhD, ABPP
The Student View: SCCAP Student Development Committee Updates
By Hong Bui & Sarah Kim
EPCAMH Journal Update
By Mary A. Fristad, PhD, ABPP
The SCCAP Conference Recap
By Mary Louise Cashel, PhD
SCCAP at APA 2025
By Kelsie Okamura, PhD & Sarah Dickinson, PhD
Science & Practice Committee Update
By Jennifer L. Hughes, PhD, MPH
Diversity Committee Update
By Juventino Hernandez Rodriguez, PhD
Membership Committee Update
By Nicole Lorenzo, PhD
Fellows Committee Update
By Martha C. (Marcy) Tompson, PhD
Distinguished Career Contributions to Science Award
Recipient: Mitch Prinstein, PhD, ABPP
Distinguished Career Award for Practice & Training
Recipient: Jonathan Weinand, PhD
Richard “Dick” Abidin Early Career Award
Recipient: Justin Parent, PhD
R. Bob Smith, III Excellence in Psychological Assessment Award
Recipient: Randall T. Salekin, PhD
Early Career Contributions to Diversity Science Award
Recipient: Roberto Luis Abreu, PhD
2025 Diversity Professional Development Awards
Eleven Winners Announced
2025 Routh Award Winners
Three Winners Announced
Student Achievement Award Winners
Six Winners Announced
2025 Student Development Committee Professional Development Awards
Five Winners Announced
AIRS SIG Update
By Elizabeth Frazier, PhD
Introducing The Autism Spectrum Disorder SIG
By Mariel Cannady, PsyD, NCSP & Allison Sallee, PhD
Bilingual Psychologists SIG Update
By Erika Garcia-Rocha, PsyD
Clinical Child & Adolescent Practice SIG Update
By Megan Lawson, PsyD, ABPP
Summer Treatment Program SIG Update
By Katie Hart, PhD & Sarah Tannenbaum, PsyD, ABPP
